It is estimated that 50 million Americans have one or more autoimmune diseases, a condition that currently has no effective treatment available, and scientists haven’t yet figured out what exactly causes it.
In this post, we will look at what autoimmune disease is, what potentially causes it, its common symptoms, current treatments, and the available clinical and anecdotal evidence as to whether the carnivore diet can treat autoimmune diseases.
Content
- What is autoimmune disease?
- Common autoimmune conditions
- Causes of autoimmune diseases
- Common symptoms of autoimmune diseases
- Current treatments of autoimmune disease
- Can the carnivore diet fix autoimmune diseases?
- Conclusion
1. What is autoimmune disease?
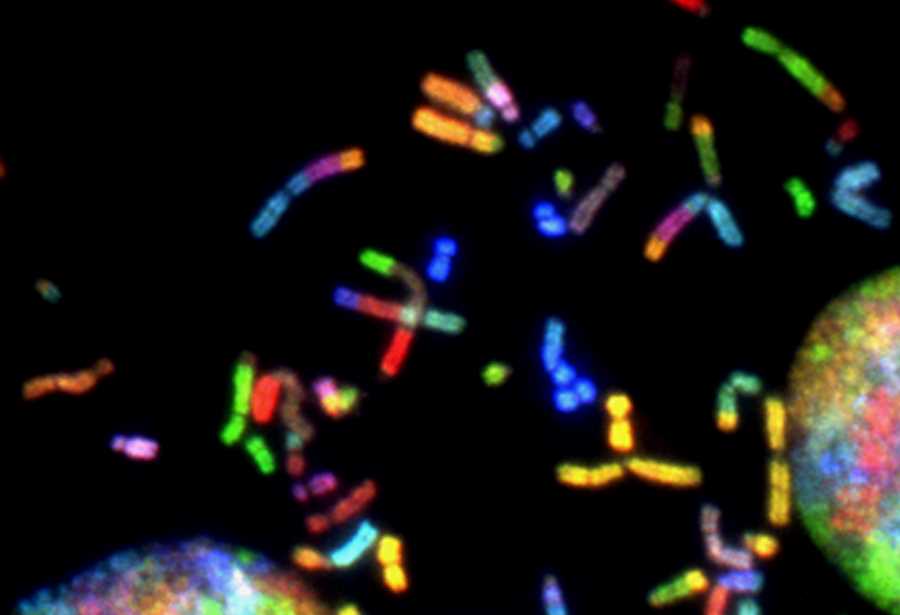
An autoimmune disease is a condition where your immune system produces antibodies that attack the body’s own cells.[1]
Your immune system is a group of cells and organs which is designed to protect your body from germs and other foreign invaders. A healthy immune system can tell the difference between ‘good’ cells that keep you healthy and ‘bad’ cells that make you sick. It should recognize bacteria, viruses, parasites, and other harmful attackers. It then marks them to be destroyed.[2]
When the immune system malfunctions somehow, it mistakenly attacks healthy cells, tissues, and organs, causing autoimmune disease.[3]
2. Common autoimmune conditions
Autoimmune diseases can affect multiple organs, a specific organ, or tissue. There are over 100 different autoimmune diseases, the most common ones are:[4, 5, 6, 7]
- Grave’s disease: an autoimmune condition that results in the overproduction of thyroid hormones
- Rheumatoid arthritis: an autoimmune condition where the immune system attacks the lining of the joints causing joint inflammation and pain
- Celiac disease: an autoimmune condition where the immune system react to gluten, causing damages to the small intestine
- Hashimoto’s thyroiditis: an autoimmune which the immune system attacks and destroys the thyroid gland, resulting in too little hormone being produced and slowing down metabolism
- Vitiligo: a condition where the skin loses its pigment cells resulting in discolored patches in parts of the body. It occurs when the cells that give your skin its color are destroyed
- Type 1 diabetes: a condition where your pancreas does not make insulin which is a hormone that helps glucose get into your cells to give them energy. As a result, blood glucose levels are too high which can lead to serious problems with your heart, eyes, kidneys, nerves, gums and teeth
- Pernicious anemia: a condition where the body is unable to properly absorb vitamin B12 to make enough healthy red blood cells
- Multiple sclerosis: a condition where the immune system attacks and destroy myelin, the fatty tissue surrounding and protecting nerve fibers. The loss of myelin forms scar tissue called sclerosis and this interferes with nerve impulses within the brain, spinal cord and optic nerves
- Glomerulonephritis: a condition where the kidneys’ filters, called glomeruli, become damaged and the kidneys slowly lose their ability to remove wastes and excess fluid from the blood to make urine
- Systemic lupus erythematosus: a condition in which the immune system attacks its own tissues, causing widespread inflammation and tissue damage in the affected organs. It can affect the joints, skin, brain, lungs, kidneys, and blood vessels
- Sjogren’s syndrome: an autoimmune condition that causes dryness in the mouth and eyes.
3. Causes of autoimmune diseases
Scientists haven’t yet figured out exactly what causes the immune system to malfunction and attack self-molecules. There are several theories, however, and they are discussed below.
Genetic risk
Genetics appears to be an important factor in autoimmune disease. For example, if a member of your family has lupus or multiple sclerosis, your risk of getting these diseases would be higher.
However, genetics is not a definite factor. You may not develop an autoimmune condition even if you carry a specific susceptible gene or multiple members of your family are affected by it.
Genetics is only one contributing factor, additional environmental triggers are needed for an autoimmune condition to develop.
It is estimated that genetic predisposition accounts for approximately 30% of all autoimmune diseases. The remaining 70% are due to environmental factors, including toxic chemicals, dietary components, gut dysbiosis, and infections which are listed below.[8]
Environment factors
Potential environmental factors that could trigger autoimmune diseases include:[9, 10]
- dietary factors: wheat, milk and a Western-style diet that is high in fat, sugar, calories, processed food and fast food
- chemical exposure: bisphenol a, mercury in fish, asbestos, nano particles, trichloroethylene (an industrial solvent known for being neurotoxic, hepatotoxic, nephrotoxic, immunotoxic and carcinogenic)
- oral pathogens: poor dental health has been linked to increase in inflammatory markers.
Nonprotein amino acids
Nonprotein amino acids are one kind of environmental trigger but they are worth mentioning separately.
Many plants produce nonprotein amino acids (NPAAs) to protect themselves against predators, pathogens, and competing plant species.[11]
NPAAs have a similar chemical structure, size, shape, and charge to protein amino acids. They are present in many plants such as legumes, alfalfa, fruits, seeds, nuts, seaweeds, and fungi. [12, 13]
Some NPAAs can be toxic to humans and animals. Some can inhibit protein synthesis while others can be mistakenly used in protein synthesis, interfere in biochemical pathways, overstimulate receptors and give rise to autoimmune reactions. [14, 15, 16, 17, 18]
When NPAAs are mistakenly used instead of a protein amino acid in protein synthesis, abnormal proteins are produced. This generates antibodies and modification of autoantigens as a mechanism to break immunological tolerance and trigger autoimmunity. Auto-antibodies formation is a characteristic of autoimmune disease. [19]
The consumption of a number of plants that contain NPAAs has been shown to have acutely toxic effects in humans. The consumption of some seeds or vegetables that contain NPAAs influences some people as a trigger for some diseases or as an exacerbating factor…
It has been observed that chimpanzees fed alfalfa and also a volunteer subject who ingested alfalfa seeds had both developed a disease with all the characteristics of lupus erythematosus … and by suppressing the consumption of alfalfa the disease disappears. [20]
Higher levels of hormones in women
Women are found to be disproportionally affected by autoimmune diseases at the rate of 2 to 1.[21]
Approximately 80% of all patients diagnosed with autoimmune diseases are women. Sjogren’s syndrome affects women in a 9:1 ratio. Systemic lupus erythematosus affects women in a 7:1 ratio. Rheumatoid arthritis affects women in a 3:1 ratio. Systemic sclerosis, an autoimmune condition affecting the skin and internal organs of patients due to a collagen defect, affects women in a 3:1 ratio.[22]
Many autoimmune disorders tend to affect women during periods of extensive stress, such as pregnancy, or during a great hormonal change and there is a theory that higher levels of hormones in women make them more susceptible to autoimmune diseases. However, this theory has not been proven. [23]
Ethnic backgrounds
Some autoimmune diseases affect different populations at different rates. For example, African-American women are at higher risk of developing lupus, scleroderma, sarcoidosis, and Sjogren’s syndrome but type 1 diabetes is more common in Caucasians.[24]
Infection and disease
Infections can initiate autoimmune diseases in animal models and later participate and facilitate the development of autoimmune diseases. The causal link has been established in the following conditions:[25]
- Antiphospholipid syndrome
- Systemic lupus erythematosus
- Rheumatoid arthritis
- Type 1 diabetes
- Multiple sclerosis.
Hygiene hypothesis
Incidence of allergic and autoimmune diseases has been rising in developed countries, whereas, in developing countries, allergy and autoimmunity are uncommon.
One theory put forward to explain this phenomenon is the hygiene hypothesis which proposes that improved hygiene, vaccination, antibiotics, and the lack of infections in developed countries may alter the human immune systems and result in inappropriate responses to innocuous substances.[26]
This hypothesis has been supported by epidemiological studies, basic immunology, animal models, and human trials of probiotic agents.[27]
4. Common symptoms of autoimmune diseases
Common symptoms of autoimmune diseases include:[28, 29]
- Fatigue
- Joint pain and swelling
- Skin problems
- Abdominal pain or digestive issues
- Recurring fever
- Swollen glands
- Hair loss
- Irritability
- Insomnia
- Itchy skin.
Each type of autoimmune disease has its own unique symptoms. For example: [30]
- Symptoms of celiac disease include abdominal bloating and pain, diarrhea or constipation, weight fluctuation, fatigue, missed periods, skin rash, and infertility
- Symptoms of type 1 diabetes include extreme thirst, urinating often, fatigue, weight loss, slow-healing sores, dry and itchy skin, tingling feeling in feet, and blurry eyesight
- Symptoms of inflammatory bowel disease include abdominal pain, diarrhea, rectal bleeding, fever, weight loss, fatigue, mouth ulcers, and painful or difficult bowel movements.
5. Current treatments of autoimmune disease
Currently, there is no cure for autoimmune diseases, only treatments to help manage the conditions. These include:[31, 32, 33]
- Drugs to relieve symptoms. For example, anti-inflammatory drugs to reduce inflammation and pain; corticosteroids to reduce inflammation; and pain-relief medication such as paracetamol and codeine
- Drugs to suppress the immune system to inhibit the activity of the immune system
- Treatment for the deficiency, for example, insulin injections in the case of diabetes or thyroid hormone replacement to restore thyroid hormone levels in people with underactive thyroid.
- Physical therapy to encourage mobility
- Surgery, for example, to treat bowel blockage in the case of Crohn’s disease.
Immunosuppressive medications that globally dampen immune responses are currently the “gold standard” of care for people with autoimmune diseases. However, these medications pose other risks such as toxicity, serious side effects, and susceptibility to life-threatening infections, and risk of malignancy. There are also new biologic drugs that target specific cells or cytokines with improved efficacy and limited toxicity.[34]
6. Can the carnivore diet fix autoimmune diseases?
What is the carnivore diet?
A carnivore is an animal that feeds on other animals. Therefore, strictly speaking, by definition, someone on the carnivore diet will basically just eat animal source food such as ruminants, pork, poultry, and seafood and drink water.
However, a broader version of the carnivore diet can include all foods that come from or are produced by an animal including ruminant meat (e.g. beef, lamb, goat, and bison), pork, poultry, seafood, eggs, dairy, and honey.
All plant foods such as fruits, vegetables, grains, legumes, seeds, and nuts are excluded from the carnivore diet.
Can the carnivore diet fix autoimmune conditions?
The carnivore diet can potentially help treat and even cure autoimmune because this diet removes an important environmental factor that triggers autoimmune conditions: troublesome food from your diet such as processed food, additives, and plant toxins.
Eliminating processed food, chemicals and additives
As mentioned above, wheat, milk, and a Western-style diet that is high in fat, sugar, calories, and processed food have been associated with autoimmune conditions.
If you suspect you have an autoimmune condition, getting rid of these potential triggering foods should be the first step.
By following a strict carnivore diet and follow healthy eating principles such as eating a variety of food and eating fresh and whole food, these potential contributing factors would be eliminated.
Eliminating plant toxins and NPAAs
Furthermore, by excluding plant-based food, you will eliminate a lot of anti-nutrients that can be found in abundance in ordinary edible plant food.[35]
You will also get rid of nonprotein amino acids (NPAAs) which have been found to initiate autoimmune conditions in animals and humans as discussed in more detail below.
While most NPAAs have low toxicity, their prolonged consumption can be toxic.
According to Bedolla et al (2021),[36] because NPAAs have a similar chemical structure, size, shape, and charge to protein amino acids, they can compete with and be mistakenly used in protein synthesis.
The replacement of protein amino acids with NPAAs results in the synthesis of abnormal or nonnative proteins that cannot function properly. This resembles a mutation in which the replacement of a single base in DNA encodes another protein amino acid in the polypeptide chain.
As the immune system identifies these abnormal proteins, it attacks those NPAAs, leading to autoimmune diseases such as rheumatoid arthritis, multiple sclerosis, psoriatic arthritis, systemic lupus erythematosus, and Sjogren’s syndrome.
It turns out your immune system is not overactive or too strong as you might have thought in this case. It just tries to do the job it is supposed to do: getting rid of substances that should not be there.
Chimpanzees fed alfalfa, which contains canavanine, a type of NPAAs synthesized by over 350 species of leguminous plants, developed a disease with all the characteristics of lupus erythematosus. A volunteer also developed lupus erythematosus while ingesting alfalfa seeds for a study of hypercholesterolemia. By suppressing the consumption of alfalfa, the disease disappeared both in the monkeys and in the voluntary subject. In addition, there were several cases of induction or exacerbation of this autoimmune condition due to the intake of alfalfa tablets.
Why you might not have heard of NPAAs before
From the evidence available so far, NPAAs seem to be a very important factor in initiating autoimmune conditions.
More than 600 different NPAAs have been identified from a wide range of plant species. For example, canavanine, a structural analog of the amino acid arginine, has been found in 1,500 species in the legume family.[37] Accordingly, NPAAs are expected to be present in many plant food people consume on daily basis.
You may wonder why not much attention has been put into this, despite the fact that autoimmune diseases cost billions of dollars every year in care. For example, according to the American Autoimmune Related Diseases Association, the estimated cost of treating autoimmune diseases in the US is greater than $100 billion annually.[38]
The answer is probably there isn’t much money to be made in telling people to eat more healthily and eliminating the root causes of their health problems. But there is definitely a lot of money to be made in manufacturing drugs to manage symptoms.
Clinical evidence on the use of the carnivore diet to treat autoimmune condition
The International Center for Medical Nutritional Intervention (ICMNI) clinic, formerly known as Paleomedicina, based in Budapest, Hungary, has been using a diet called the paleolithic ketogenic diet (PKD) to treat many chronic conditions including autoimmune conditions since 2012.[39]
Previously they had been using the paleolithic diet which was proven to be ineffective in the vast majority of chronic conditions. They then developed the paleolithic ketogenic diet based on clinical evidence from around 4000 patients.
Their view is that eating fruits and vegetables does not form part of our physiological needs but is associated with risks. Plant foods can only be regarded as ”relatively” safe and only when certain plant food items are consumed and only in limited amounts.
In the sections below, we will look at the specifics of the paleolithic ketogenic diet used by the ICMNI before looking at their clinical results.
The paleolithic ketogenic diet
The paleolithic ketogenic diet is a high-fat animal-based diet with a fat-to-protein ratio of about 2:1 in weight. It has a continuum starting with 100% animal-based food and allowing for up to 30% plant food.

However, according to Dr. Zsofia Clemens, a neurobiologist and clinical researcher working at the ICMNI, this does not mean they are recommending plant food at all for any reason. This is just an allowance for those people with not so severe conditions who can physiologically tolerate plant food.
If they have a patient with metastatic cancer, a patient who underwent several cycles of chemotherapy, or a patient with an autoimmune condition, then there is no question that he or she will need to be on a full animal-based high-fat diet with just meat, fat, and organ meat.
Though they would love to please their patients and allow some flexibility, that would not be in the best interest of the patients. For some patients, there is no choice but to strictly adhere to an animal-based diet.
If they have a patient with hypothyroidism without complications or just a simple overweight patient, a simple type-2 diabetes patient, then he or she may be doing well with a diet that allows for some vegetables and fruits.
Further details on the diet are:
- Animal foods include red and fatty meats, fat and offal preferably from pasture-raised animals
- Fat to protein ratio about 2:1 (in grams). Dr Zsofia Clemens mentioned that the basic recommended ratio is 100 grams of average meat and 35 grams of animal fat
- No nitrates, nitrites, or other additives in meat products
- Plant foods only include fruits and “paleolithic”vegetables from organic sources
- No artificial sweeteners but honey is allowed in moderation
- Black and herbal tea are excluded
- Coffee is allowed only after full regeneration and in moderation
- Eggs are initially excluded in those with highly elevated intestinal permeability and/or vaccines during the preceding 6 months.
In summary, the paleolithic ketogenic diet is a clean animal-based high-fat diet to ensure patients stay in ketosis. Plant food is not recommended but allowed in certain patients who can tolerate it.
Clinical results using the paleolithic ketogenic diet
Below are only successful cases that have been published.
1. Type 1 diabetes mellitus (2014)[40]
A 9-year-old child had a three-month history of polyuria, polydipsia, polyphagia, fatigue, and weight loss. His abdomen was bloated. He had frequent upper respiratory tract infections, epistaxis, and eczema on his hands as well as asthma. He was diagnosed with type 1 diabetes and was initially was on an insulin regime with a high carbohydrate diet.
He was advised to follow the paleolithic ketogenic diet consisting of only animal meat, fat, offal, and eggs with a fat-to-protein ratio of about 2:1. Following this advice, the child consumed meat, fat, and offal only from cattle and pork. He did not consume vegetables and fruits at all. Artificial sweeteners and vegetable oils were excluded. He was allowed to consume small amounts of honey. The diet was introduced gradually within five days.
Following this dietary change, glucose levels normalized and he was able to discontinue insulin. No hypoglycemic episodes occurred on the diet and several other benefits were achieved including improved physical fitness, reduction of upper respiratory tract infections, and eczema. At the time of reporting, he had been on the diet for 19 months.
2. Type 1 diabetes mellitus (2014)[41]
A 19-year-old male with newly diagnosed T1DM. The patient was first put on an insulin regime. Twenty days later, he shifted towards the paleolithic ketogenic diet and was able to discontinue insulin. Strict adherence to the diet resulted in normal glucose levels and a more than three-fold elevation of C-peptide level indicating restored insulin production. At the time of reporting, the patient had been on the paleolithic ketogenic diet for 6.5 months. He was reportedly free of complaints, and no side effects emerged
3. Crohn’s disease (2015)[42]
A 14-year-old boy presented with fatigue, low-grade fever, iron deficiency anemia, lower abdominal tenderness and perianal dermatitis. He was diagnosed with Crohn’s disease.
The paleolithic ketogenic diet was recommended and the diet is consisting of animal fat, meat, offal and eggs with an approximate 2:1 fat to protein ratio. Red and fat meats instead of poultry as well as regular intake of organ meats from pork and cattle were encouraged.
This resulted in resolution of symptoms, normalized laboratory parameters as well as gradual normalization of bowel inflammation. The patient was able to discontinue medication within two weeks. At the time of reporting, he had been on the diet for 15 months and is free of symptoms as well as side effects.
Anecdotal evidence on the ability of the carnivore diet to treat autoimmune condition
Many people have reported on social media of their success in using the carnivore diet to treat their autoimmune conditions. Below are a few examples that I found on the web.
Mikhaila Peterson [43]
Mikhaila Peterson was diagnosed with juvenile rheumatoid arthritis at the age of 7. The condition was so severe that she was put on multiple immune suppressants. At the age of 17, she had hip and ankle replacements.
Mikhaila also had symptoms of depression, anxiety, and OCD tendencies from age 9 and later on was put on SSRI (selective serotonin reuptake inhibitors), a widely used antidepressant.
Mikhaila had other health issues including fatigue, rashes, itchy skin, brain fog, and had to take more and more medications.
Through research and trial and error, she came to the carnivore diet which for her was just meat, salt, and water. But, according to her, the carnivore diet has allowed her to get off over 10 medications and put several, seemingly incurable, life-long diseases into complete remission, including arthritis, depression, bipolar type II, idiopathic hypersomnia, Lyme disease, psoriasis, and dyshidrotic eczema.
The Armstrong sisters [44]
Ashley Armstrong and Sarah Armstrong from Central Illinois were diagnosed with autoimmune conditions about 10 years ago.
They tried many different diets, from plant-based, fasting, keto to macro-based eating, and then went on a year of the carnivore diet. They said that the carnivore diet had cured their autoimmune condition and other health problems including constipation, bloating, depression, fatigue, brain fog, circulatory problems, and Raynaud’s syndrome.
At the moment, they are animal-based but no longer exclusively carnivores.
Georges St-Pierre [45]
George St-Pierre or GSP is a Canadian professional mixed martial artist and UFC world champion. He has ulcerative colitis, a chronic inflammatory bowel disease condition that results in inflammation and ulcers on the inner lining of the colon and rectum. He also has arthritis on one of his big toes.
He tried the carnivore diet for a month under the guidance of Dr. Paul Saladino and both of these conditions improved.
Chad Mendes [46]
Chad Mendes is a retired American professional mixed martial artist who suffers from psoriasis. This is an immune-related disease that causes inflammation in the body resulting in red, itchy scaly patches, most commonly on the knees, elbows, trunk, and scalp.
He was told by two different dermatologists that diet has no effect on psoriasis. However, after nearly two months on the carnivore diet, he experienced remarkable improvements, the red scaly patches on his legs had mostly healed.
Joe Rogan [47]
Joe Rogan is a well-known American comedian, podcaster, and mixed martial arts commentator. Joe Rogan did only one month of carnivore diet trial in January 2020. Rogan has vitiligo, a condition where the skin loses its pigment cells resulting in discolored patches in parts of the body. Rogan said that bunches of white spots went away by the end of the experiment.
Testimonials on YouTube[48]
“I have multiple sclerosis. I went carnivore 11 weeks ago. I’m off of every supplement I used to take, every prescription drug, and I had an appointment with my specialist today – despite three lesions on my spine and a brain that looks like swiss cheese on an MRI, I am completely symptom-free. I was smiling and lively in a way the doctor had never seen me and he remarked, it was as if he was only meeting me for the first time today. I refused the next Rituxan infusion. It’s amazing what can happen when you feed your DNA what it expects from its environment”
“Diverticulitis…my twin sons are 39 yrs old and they learned by trial and error trying different diets and discovered that eating basically carnivore has changed their life dramatically…also eating organic grass-fed beef…if they stray too far from carnivore, they suffer immensely”
I started this carnivore way of eating 3 weeks, and 2 days ago. I’ve lost about 10 pounds, and my arthritic knees have drastically improved. I have more energy and feel much better
Carnivore for over 2 years. Celiac & Duhring’s disease, PHP (with an autoimmune component), and adenomyosis symptoms have either been eliminated or lessened through animal-based eating and fasting.
I did 16 months Keto and in February this year I began carnivore. I’m celiac, had high blood pressure and rheumatoid arthritis. Since I have been eating carnivore I have no arthritic pain, celiacs is getting better and I feel my blood pressure has improved
IBS, Hashimotos, multiple sclerosis and I am doing so much better now. I’ve been carnivore for two years… won’t ever go back to eating veg or carbs.
I started Carnivore in November 2019 coming from a strict keto diet, I have 6 autoimmune illnesses that have plaqued me since I was 12 years old, some were acquired lately in life. Now at age 52 on strict Carnivore I am feeling better than I can remember in years. I have rhuemetory arthritis, ankylosing spondylitis, Candida, celiac disease, IBS, sjogren’s syndrome, with all of that I was 280 Lbs. now Im down to 185 Lbs. I am no longer in constant pain, no more knee pain, joint pain. With bad advice from many doctors over the years I took Prilosec for 22 years and anti inflammatory meds from my arthritis doctor, and many other prescription drugs, all of which could have been avoided.
Conclusion
The current view of the general medical profession is that there is no effective cure for autoimmune diseases, only treatments to help manage symptoms and improve the quality of life for patients.
The so-called “gold standard” of care for autoimmune patients at the moment is giving patients immune-suppressing drugs. As a good immune system is your best defense against viruses, bacteria, and other outside invaders, suppressing it means weakening your self-defense and can bring in a whole host of other problems.
Clinical evidence and anecdotal evidence indicate that there may be a better way to manage or even cure autoimmune conditions: the carnivore diet.
The carnivore diet can meet all your physiological needs while eliminating some potential root causes of autoimmune conditions.
If you think you might have an autoimmune condition, please talk to your doctor if you haven’t done so already.
If you have tried other conventional approaches and been told that there is no cure, based on my own research on this topic, I strongly suggest you give the carnivore diet a go.
And if you do like to try it out and see if it can improve your health, I’ve written a detailed guide on how to start the carnivore diet here. Please check it out, it will definitely save you a lot of time.
Disclaimer: The information in this post is for reference purposes only and not intended to constitute or replace professional medical advice. Please consult a qualified medical professional before making any changes to your diet or lifestyle.